Commonly Asked Questions About Childbirth Answered
Twenty-one frequently asked questions/answers concerning birthing procedures and vaccines
Donna Young
Box 504 P.O.
Dawson Creek, BC
Canada V1G 4H4
Phone: +1 250 782 9223 or Toll-free: +1-877 782 9223
Email: [email protected]
Gary S. Goldman, PhD
Box 847 Pearblossom, CA 93553
Phone: +1 661 944 5661 Fax: +1 661 944 5661
Email: [email protected]
Website: http://www.medicalveritas.com/
Do You Want to Remain Informed about the Latest Vaccine News?
1. Question: What is Active Management of Labor?
Answer: Active Management of Labor, or AML, is a protocol that manages a woman’s birth—often causing a shorter time of labor, and hence, benefiting the schedule of a busy physician and/or hospital staff. Over the years, the labor stage has been drastically reduced from as much as 36 hours in the 1950s, to 24 hours in the 1960s, to less than 12 hours through use of drugs in the 1970s when AML was introduced. Narcotics, such as Demerol® (or pethidine) are used for pain relief and tend to slow down labor; while other drugs, such as oxytocin (Pitocin®) accelerate the labor. Often fluids and drugs are administered intravenously through an IV to help prevent dehydration and control the progression of labor.
Because oxytocin is naturally produced in the body, physicians may utilize this fact to persuade the mother to begin supplemental oxytocin administration. The healthcare provider may attempt to mislead the mother to accept such treatment based on the reasoning that oxytocin is simply a natural hormone that triggers milk release from breast tissue when infants nurse and causes muscle contractions in the uterus during labor. The man-made oxytocin may contain chlorobutanol, a preservative, which may lead to thyroid-related metabolism problems. AML utilizes customary hospital procedures that hasten labor: pitocin, amniotomy (breaking the waters), forceps, fundal pressure, cord traction in 3rd stage, etc.; whereas, at home, labor progresses at its own natural pace without such interventions. The superior outcomes of the home birth group would suggest that the philosophy of hospital obstetrics to rush and shorten labors is not in the best interest of the mother or the baby’s safety. The study results are given in Table 1.
One of the largest scientific studies comparing the outcomes of homebirth with hospital birth was done by Dr. Lewis Mehl and Associates. This study compared the outcomes of matched populations. In the study, 1,056 homebirths were compared with 1,046 hospital births in the U.S. For each home-delivered patient, a hospital-delivered patient was matched for age, length of gestation, parity, risk factor score, education and economic status, race, presentation of the baby, and individual major risk factors. Both groups had trained birth attendants and received regular prenatal care.
According to Dr. Sarah Buckley, writing in the book by Shivam Rachana, (Greenwood Press, Yarra Glen, 2000), “Choosing to forego preventative oxytocics, to clamp late (if at all), and to deliver the placenta by our own effort all require forethought, commitment, and that we choose birth attendants that are comfortable and experienced with these choices.”
Delayed clamping results in many benefits, including less blood retained in the placenta, thus allowing easier birthing of the placenta in the third stage of labor.

This photo shows the difference between a prematurely clamped and a delayed clamped baby:

Table 1. Results from the study of Dr. Lewis Mehl and Associates

2. Question: The doctor has told me: “If the baby is not here by such and such a date, I am going to induce labor.” I am so uncomfortable, so will this benefit me?

Answer: Women are usually offered induction when they are more than 2 weeks overdue (“postdates”). Research suggests that there may be a very small extra risk of problems for post-dates babies, but induction also has risks. The drugs used can cause very strong contractions, necessitating strong pain relief such as epidurals (which has risks for mother and baby). Strong contractions can compromise blood supply to the baby, causing fetal distress. An induced birth will involve more drugs and procedures and a higher chance of cesarean, especially for first-time mothers. The long-term effects of induction have not been well studied.
3. Question: What is the PKU test?

Answer: The PKU is a screening test (not a diagnostic test) usually done by a needle stick in the heel of the newborn. Phenylketonuria (PKU) is an inherited metabolic disease whose characteristic feature is a person’s inability to break down excess amounts of the amino acid phenylalanine (Phe). PKU is caused by a defective gene which cannot make enough of an enzyme called phenylalanine hydroxylase (PAH). If there is no family history of this metabolic disease, some question the validity of testing. It is a common practice, however, to also simultaneously screen for congenital hypothyroidism (CH) and other thyroid functions.
4. Question: Why are antibiotic ointment and silver nitrate
placed in the eyes of a newborn?

Answer: The practice of placing antibiotic solution/ointment in the eyes of a newborn shortly after birth is common throughout the world and mandated by law in many states. The reason for this practice is to prevent infection of tissues surrounding the eyes caused by bacteria (especially due to sexually transmitted diseases) which may be present in the birth canal as the baby is being born. The infant has a significantly lower risk of getting an eye infection whether that be from a common bacteria or sexually transmitted one; however the risk of inflammation of the tissue around the eye for a couple of days is increased. Alternatively, since erythromycin ointment causes less irritation, you may desire to discuss use of this antibiotic option with those caring for the baby following birth.
5. Question: Why is a vitamin K injection given to a newborn?

Answer: In the U.S., the standard of care as recommended by the American Academy of Pediatrics is to give Vitamin K by injection within the first few hours after birth. Newborns initially have low levels of vitamin K. However, low levels (relative to those levels in an adult) of vitamin K in newborns is normal. Vitamin K is used as a prophylactic measure to prevent late-onset hemorrhagic disease (HDN). Late onset HDN occurs at a rate of 4 to 19 per 100,000 babies without supplemental Vitamin K. In babies who receive a Vitamin K injection, the rate is less than one to two in 400,000. Since HDN is a relatively rare problem, many parents now choose for their babies not to have such an injection. Some infants have died of HDN despite vitamin K prophylaxis [Morrice LM, Jagdis FA et al. Case report: fatal hemorrhagic disease in a newborn despite vitamin K prophylaxis. Can Fam Physician 1998 Sep.;44:1893-1894].
Other studies suggest oral vitamin K therapy is effective [Clark FI, James EJ. 27 years of experience with oral vitamin K1 therapy in neonates. J. Pediatr. 1995 Aug.;127(2):301-304;
Huysman MW, Saver PJ. The vitamin K controversy. Curr Opin Pediatr. 1994 Apr.;6(2)129-134]. An oral vitamin K preparation Konakion MM, given in 3 doses of 2 mg at birth, 7 days, and 30 days of life yields higher plasma vitamin K concentrations than a single injected dose at birth [Greer FR, Marshall SP et al. A new mixed micellar preparation for oral vitamin K prophylaxis: randomised controlled comparison with an intramuscular formulation in breast fed infants. Arch Dis Child. 1998 Oct;79(4):300-5]. The administration of the birth dose is difficult and may not be effective since the infant does not have the necessary enzymes to synthesize Vitamin K. Konakion MM, manufactured by Roche Pharmaceuticals, contains lecithin and glycocholic acid; vitamin K requires emulsification and the presence of bile salts to aid absorption.
6. Question: How can I prevent my baby from being administered the Hepatitis B vaccine, Hepatitis A vaccine, and vitamin K injection?

Answer: For those who are planning a hospital birth but want to evade invasive routine post natal procedures such as a Hep B shot, Hep A shot, and vitamin K injection, a very specific birthing contract must be submitted to the hospital in advance of the birth. Hospital staff must be informed, in advance, of your needs, wants and desires where your baby and birthing experience are concerned.
7. Question: Should Active Management of Labor (AML) be
avoided?
Answer: Yes. AML is not a natural procedure and investigation reveals its main objective is to manage birth by time convenience, thus resulting in higher profits to medical institutions. Rarely does AML serve the interests of the mother or the infant. AML uses drugs to delay or quicken labor. It uses flat-on-the-back and semi-sitting birth positions that yield some advantage to the attending physician but disadvantage the woman by closing her birth canal up to 30%. This results in a more painful birth and increased stress to the infant. When
drugs are used, the umbilical cord is early clamped to prevent the drugs from crossing the placenta and causing harm to the child. In some cases, the placenta blood and the cord blood are being harvested for the hormones and enzymes that should have otherwise transferred into the child to assure the child is not in a weakened condition. AML is often followed with control over the child, including administration of the Hepatitis B vaccine, and later the rotavirus vaccine, and many, many others.
8. Question: Should a woman consider birthing in her home without a professional or certified medical person present?
Answer: The woman has a right to decide which medical protocols she will accept and reject, even if these protocols lead to her or her child’s death, but to be wise, a woman should always have someone to assist her. The birthing mother could become unconscious and both the mother and child could die if the mother is bleeding or the child requires emergency aid. The mother should have an attendant who is both comfortable and experienced with natural birthing options desired by the mother.
9. Question: If the cord is wrapped around the baby’s neck
(called nuchal cord), should the cord be cut?
Answer: No. For an umbilical cord around the neck, it is best and the optimal practice to place a soft object between the neck and the cord, rather than to tie the cord in two places and cut the cord. This soft object (finger or sponge) is to prevent neck and vocal chord injuries. When the infant is fully birthed, simply, unwrap the lifeline and let the untied lifeline continue infusing blood into the baby’s expanding lungs. A stronger, healthier and living baby will result.
It has been noted that the infant can go into shock when deprived of just 20% of its blood volume. In a legal case involving an infant named Chow, the cord was wrapped around the child’s neck and was clamped and cut. Despite efforts to resuscitate, the child experienced hypoxic brain damage that lead to his becoming blind and mute, a quadriplegic, and having cerebral
palsy [Chow (Litigation guardian of) v. Wellesley Hospital, 1999 O.J. No. 279, DRS 99-03087, Court File No. 92-CQ-017535]. Immediate cord clamping can deprive an infant of up to 60% of its total blood volume resulting in a struggle to keep the child alive and healthy. Thus, clamping and cutting of the umbilical cord should not be done until after the birthing of the placenta. Prematurely clamping/cutting of the umbilical cord is an intervention that has been associated with hypovolemia, anemia, shock, hypoxic-ischemic encephalopathy, and cerebral palsy [Simon EN, Morley GM. Review–Birth brain injury: etiology and prevention—Part III: Concealed and clandestine trauma. Medical Veritas 2005 Nov; 2(2):513-520].
10. Question: What if the physician or hospital insists on keeping the cord and/or placenta?

Answer: This request is likely made for purposes of monetary gain and economic enrichment since the hospital/physician can market these biological products to research centers and blood banks. Specify clearly in a birth contract that the placenta, cord, and baby are to remain as a complete unit.
11. Question: I am experiencing excruciating back pain (back
labor). What can be done?
Answer: If the baby is not well positioned, or turned with the back of the head against your spine, this can cause extreme back pain. A scan may be needed with a professional determination regarding the location of the placenta. Placenta previa is a condition in which the placenta in the womb is blocking the birth canal exit. This may require a C-section. C-sections should only be for emergency purposes, as they are considered a major operation that carries higher risks to both mother and child compared to a natural birth choice [Villar J, Carrolli G et al. Maternal and neonatal individual risks and benefits associated with caesarean delivery: multicentre prospective study. BMJ 2007 Oct 30].
There are a number of different approaches to alleviating back labor, some of which include:
(1) change positions,
(2) walk around,
(3) sit in a chair,
(4) get on all fours and sway your hips back and forth,
(5) lay on your side in a fetal position and round your back,
(6) apply heat or cold, and
(7) massage the sore area.
12. Question: The healthcare provider wants to intentionally break my waters (called amniotomy). Should I permit this?

Answer: No. This procedure is unnatural and yet the most commonly performed to supposedly speed up labor and shorten contractions. Associated risk factors include dry birth where the baby may not turn naturally in the birth canal—producing a more painful birth experience for the mother and creating more stress for the child. Sometimes water may gush out with such force that the cord is born first. When this occurs, the child may compress the cord, interrupting fetal circulation whereby oxygenated blood is infused into the infant’s lungs. When the waters are not broken, there exists a protection against harmful bacteria that may be present in the mother’s birth canal and a natural cushion for the baby’s delivery [Smyth R, Alldred S et al. Amniotomy for shortening spontaneous labour. Cochrane Database Syst Rev. 2007 Oct 17;(4):CD006167].
13. Question: After many hours of labor, I have only dilated a few centimeters and am not progressing. Should I allow the physician to administer a low dose of oxytocin (Pitocin)?
Answer: No, this is the same drug used to accomplish abortions. When oxytocin is added to your own oxytocin supply, it can enhance labor pain, cause closer, longer duration contractions, and may result in earlier separation of the placenta from the uterine wall. In this case, the baby can begin to start suffocating in the womb. Avoid drugs by planning for a warm water birth and drink hot tea. Both of these approaches will help you to relax and start birth labor naturally, without risk to you or your baby. Oxytocin is man-made and may contain a preservative called chlorobutanol. This has caused immediate adverse effects such as a drop in maternal blood pressure [Rosaeg OP, Cicutti NJ et al. The effect of oxytocin on the contractile force of human atrial trabeculae. Anesthesia & Analgesia 1988; 86:40-44] and can cause later side effects, attacking both the infant’s and the mother’s thyroid. Only years later, may hyper-or hypo-metabolism activity develop. Avoid oxytocin and any other trade name drugs that are substituted for it. It is used for time efficiency to reduce the time the mother is in the hospital.
Consider the option of going through labor at home. Some women choose a friend’s home to labor near the hospital vicinity, and when close contractions become regular, you are taken to the hospital to arrive in time to give birth with little medical intervention—often best for mother and child.
14. Question: Can I drink liquids while in labor?

Answer: Yes. It has been suggested that water or herbal tea, as hot as can be sipped without burning your mouth, can be beneficial since it can relax you and thus, may hasten the progression of a more natural birth. Alcohol should be avoided as should herbal teas to which you are allergic. There are a variety of teas that are known to specifically speed up labor and/or prevent excessive bleeding. In one limited study of small sample size, it was found, “Raspberry leaf, consumed in tablet form, was found to cause no adverse effects for mother or baby, but contrary to popular belief, did not shorten the first stage of labor. The only clinically significant findings were a shortening of the second stage of labor (mean difference = 9.59 minutes) and a lower rate of forceps deliveries between the treatment group and the control group (19.3% vs. 30.4%).” [Simpson M, Parsons M et al. Raspberry leaf in pregnancy: its safety and efficacy in labor. Journal of Midwifery and Women’s Health 2001;46(2):51-59].
15. Question: What is the maximum time an umbilical cord has continued to pulsate following birth of the infant?
Answer: Dr. Mavis Gunther published research that indicated drugged infants had pulsating umbilical cords for up to 20 minutes when the baby was kept in a warm environment
[Gunther M. The transfer of blood between baby and placenta in the minutes after birth. Lancet, 1957 Jun 22;272(6982):1277-1280]. Physicians who perform immediate cord clamping have not given adequate time for full placental transfusion of blood and may have put the child in harm’s way. The completion of the birthing process includes the 3rd stage of labor—when the placenta is expelled. The child should be immediately wrapped to maintain warmth. It is not ethical for a hospital to seek monetary enrichment by cutting the cord, only to sell the cord and placenta to research institutions, blood banks, and cosmetic corporations.
16. Question: Has active management of labor (AML) been considered as a successful strategy for other countries to adopt?

Answer: No. Doris Haire, presented a report of her research at the Birth Without Borders Conference, sponsored by UNICEF, in Chiang Mai, Thailand, March 1, 1997. Doris Haire, President of the American Foundation for Maternal and Child Health, New York, began her speech by stating:
“It is painful for me to report that nowhere in the world has the normal physiology of childbirth been more distorted than it has in the United States. There is growing concern in the U.S. that obstetric related drugs, which you refer to as medications, contribute
significantly to our embarrassingly high rate of learning disabled children. American children, in general, continue to lag behind most industrialized countries in academic achievement, especially in those aspects of education, such as math and science that require comprehension and deduction. Despite hundreds of millions of dollars spent each year on prenatal care and
high tech maternity care U.S. schools continue to be flooded with children who cannot learn without special education instruction by teachers trained to work with learning impaired children. Special education has become a growth industry in the United States. And while we would be more comfortable blaming the problem on our high rate of prematurity, the fact is, that 75% of all handicapped children in the U.S. were born within the normal range of gestational age and weight, with no predisposing familial condition. Before your obstetric services are tempted to adopt the westernized approach to maternity care help your colleagues to realize that the interventions that have become so much a part of westernized maternity care have the potential for permanently harming both the mother and her baby and eventually the fabric of society.”
17. Question: Why are some parents not informed or are only informally told that the newborn infant is to be given a Hepatitis B vaccine?

Answer: The administration of the Hepatitis B vaccine is currently viewed as a matter of routine care or treatment. Therefore some healthcare professions do not feel obligated to inform the parent regarding administration of the vaccine. The mother or parents should instruct the physician and healthcare staff that the child is not to receive the Hepatitis B vaccine. Please see next question if you are further pressured to accept the Hepatitis
B vaccine for your child.
18. Question: My doctor is pressuring me to have my baby vaccinated. What should I say to him?

Answer: A quick response might be, “I would like to postpone vaccination until a later time.” Another response might be, “I have researched the adverse effects associated with the Hepatitis B vaccine. I and other peer-reviewed medical research support the fact that the vaccine poses more risk than benefit since Hepatitis B can only be contracted from a mother who is positive for Hepatitis B, or through sexual contact, or intravenous drug use. Therefore, I am making the informed choice of not having my child vaccinated with the Hepatitis B vaccine.”
As another alternative, virtually all 50 states in the U.S. allow a medical exemption and some provide a religious and/or philosophical exemption from vaccines.
19. Question: Are there established medical policies and/or bulletins that actually put an infant in harm’s way?
Answer: Yes, the Society of Obstetricians and Gynecologists of Canada, SOGC, promoted immediate cord clamping in Policy #89 of May 2000 when their Policy #71 of December 1998 indicated they were fully aware that early cord clamping contributed to babies developing an anemic condition and having a shortage of blood of up to 50%. Another influential group, the American College of Obstetricians and Gynecologists (ACOG), delayed in cancelling their bulletin #216 of November 1995 despite objection by one of its members. Finally, the policy was cancelled in 2002; however, ACOG, SOGC, and other educating organizations are remiss in failing to make a public statement regarding the negative consequences of early cord clamping.
Another organized control group is the Federation of International Gynecologists and Obstetricians (FIGO). Their first ever joint policy with the International Midwives opted for use of early umbilical cord clamping as a precaution for fear of excessive bleeding of the mother. In fact, many organizations support the induction or augmentation of labor through use of oxytocin. The administration of labor-inducing drugs necessitates immediate cord clamping since these drugs cross the placenta, adversely affecting the infant. Mothers are rarely informed of the adverse effects and negative consequences of such labor management—including the need to resuscitate the infant due to low blood volume and pressure. The subsequent anemic condition in the child can persist for months.
20. Question: Have there been any known instances where infants have experienced serious illness or have died following a vaccination?

Answer: Yes. The U.S. government maintains a database and has in place VAERS, the Vaccine Adverse Event Reporting System. Unfortunately, reporting of adverse events by physicians is not mandatory and it is estimated that the VAERS data-base contains only from 1% to 10% of actually occurring adverse reactions. With regard to the reporting in VAERS, it is true that causality is rarely proven; however, the timing of an adverse event closely following a vaccination and lack of any other obvious cause are most often the only criteria of potential significance for a suspected adverse reaction to a vaccine. Since physicians believe vaccines are entirely safe, parents are not alerted to the deleterious effects that might ensue, so association of a medical condition with vaccination often goes unnoticed. A large variety of adverse reactions and some deaths have been associated with vaccines for Hepatitis B, Varicella, and other diseases.
In some instances, what is reported as Sudden Infant Death Syndrome (SIDS), is actually death due to vaccination. In cases involving Shaken Baby Syndrome (SBS), where parents or caretakers have been accused of shaking their baby to death, toxicological investigations have shown bleeding and subsequent death due to vaccinations. Additional references on SBS include the following: Nicholls LD. Daubert hearing regarding Shaken Baby Syndrome. Medical Veritas 2006 Nov; 3(2):1220-1226; Buttram HE. Shaken baby syndrome (SBS): general commentary. Medical Veritas, 2004 Apr;1(1):31-33; and Al Bayati MA. Shaken Baby Syndrome or medical malpractice? Medical Veritas 2004 Apr.;1(1):117-129.
Vaccines can have a long-term effect on the immune system of the individual they are administered to; however, the long-term negative effects of vaccination are often never considered. For example, following the adoption of the universal Hepatitis B vaccination campaign in France which started in September, 1994, there was an increase in the number of children with vaccine-induced multiple sclerosis and autoimmune diseases [Girard M. When evidence-based medicine (EBM) fuels confusion: multiple sclerosis after hepatitis B vaccine as a case in point. Medical Veritas 2007 Nov.;4(2):1436-1451].
21. Question: Why isn’t delayed cord clamping standard practice if it means healthier babies and has no adverse effects?

Answer: Contrary to what some physicians have been taught, research indicates there is no significant maternal postpartum blood-loss volume associated with delayed clamping. The concerns in the newborn of increased blood volume and red blood cell volumes overloading the heart and causing respiratory difficulties is unfounded when cord clamping is delayed. Some physicians recommend immediate or early cord clamping believing that there is greater risk of jaundice. However, studies indicate bilirubin levels were not related to
the time of cord clamping. A delay in cord clamping of just two to three minutes has yielded benefits to the newborn that include
(a) increased levels of iron,
(b) lower risk of anemia,
(c) less transfusions necessary, and
(d) less risk of intraventricular hemorrhage.
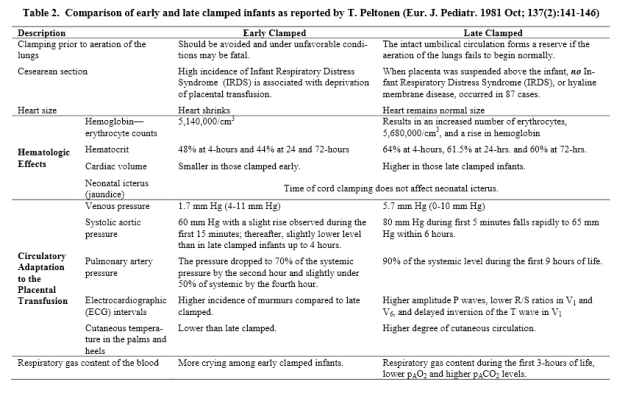
The highlights from the research of T. Peltonin are given in Table 2 below [Peltonen T. Placental Transfusion — Advantage and Disadvantage. Eur. J. Pediatr. 1981 Oct; 137(2):141-146].
Summary: Past studies have shown that some health benefits accrue to both premature, full-term, and even C-sectioned infants when clamping and cutting of the umbilical cord is delayed only 30 seconds to 2 or 3 minutes. Yet, the health of these infants was still compromised relative to infants that had no clamping or clamping and cutting only after birthing of the placenta. A truly informed mother and a signed birth contract that specifies no cosmetic cutting of the cord and use of appropriate birthing positions is optimal. These choices prevent putting either the mother or the infant in harms way. The past and present empirical medical facts (visual, testable, and measurable) are known to minimize the risk of blood infection to the infant or other weakening of the infant’s internal cells, organs,
muscles, heart, nervous system, and respiratory system.
Only by allowing the birthing process to proceed naturally with the mother’s informed participation in the choices and management of her infant’s birth, will we likely see a trend toward the birthing of healthier infants—no longer putting mother and infant needlessly in harm’s way.
Table 2. Comparison of early and late clamped infants as reported by T. Peltonen (Eur. J. Pediatr. 1981 Oct; 137(2):141-146)
—————————————————-

Please sign and share Donna Young’s PETITION
—————————————————
RELATED ARTICLES
Cord clamping
– Cord clamping and stem cell collection – by Hilary Butler
– How Early Umbilical Cord Clamping Damages Babies’ Brains
– The Importance of Delayed Cord Clamping
Hepatitis B vaccination
– Hep B vaccine for new babies – WARNING: SHOCKING PHOTOS!
Breastfeeding
– Breastmilk Is Not Just Food – by Hilary Butler
INFORMATION ABOUT EXEMPTIONS FOR BIRTH (AND SCHOOL):
– www.vaclib.org/exemption.htm
First Baby Bath
– Don’t remove the vernix!
https://www.vaccinationinformationnetwork.com/dont-remove-the-vernix/
– 6 Reasons to Delay Baby’s First Bath
RESOURCES
Books

Gentle Birth, Gentle Mothering: A Doctor’s Guide to Natural Childbirth and Gentle Early Parenting Choices – Sarah J Buckley
Educational videos

Download the wonderful documentary ‘Birth Into Being’ by Elena Tonetti-Vladimirova for only US$12
———
Healthy Happy Child Childbirth Education DVD Series
———-

– Delaying Your Baby’s Bath Has Benefits
———-









